- 1-866-599-3376
- Patient Portal
- Pay A Bill
- Newsletter: Vancouver Salem Astoria Gresham Longview
- Specialties
- Providers
- Resources
- Locations
- Careers
- Contact
- Search
Thirty million Americans suffer from venous disease, the most common being Venous Insufficiency. Unfortunately, most people suffering from venous disease have never even been evaluated. Often their primary care provider has told them not to worry about their vein symptoms, or that they are only cosmetic. Patients may also believe (or have been told) that the treatment is worse than the disease. (It’s not!)
For most patients, varicose veins are the first hint that there is something wrong. If these abnormal veins are ignored, a condition called Chronic Venous Insufficiency (CVI) will develop. CVI is a progressive medical condition that worsens over time and affects the low pressure vessels in the legs that carry oxygen-poor blood back to the heart. The phases of the disease are a direct result of an abnormal increase in venous pressure. This increased venous pressure, if left unchecked, will result in a cascade of events that will lead to the advanced stages of CVI.
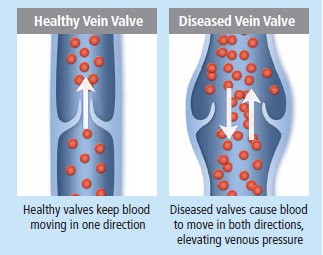 Healthy veins contain valves, which are composed of gossamer-thin flaps of tissue that open and close as part of their function to return blood back to the heart. In concert with the muscles in the leg, the valves allow blood to flow upward, against gravity. Venous reflux, which is the underlying malfunction and underlying cause of CVI, occurs when the valves become damaged or diseased. Reflux – or backward flow of blood- occurs in these affected veins. Because normal valves are critical for the proper functioning of these low pressure vessels, these veins become incompetent and cannot do their job. Pooling of blood, which leads to venous hypertension, is the end result.
Healthy veins contain valves, which are composed of gossamer-thin flaps of tissue that open and close as part of their function to return blood back to the heart. In concert with the muscles in the leg, the valves allow blood to flow upward, against gravity. Venous reflux, which is the underlying malfunction and underlying cause of CVI, occurs when the valves become damaged or diseased. Reflux – or backward flow of blood- occurs in these affected veins. Because normal valves are critical for the proper functioning of these low pressure vessels, these veins become incompetent and cannot do their job. Pooling of blood, which leads to venous hypertension, is the end result.
Varicose veins become a chronic problem when the symptoms and signs are severe enough to interfere with the enjoyment of an active life style. By the time a person develops significant swelling and or skin changes, the diagnosis of Chronic Venous Insufficiency is a foregone conclusion.
WHAT CAN I DO?
Most importantly, if you think you have symptoms of venous insufficiency, no matter how mild, you should consult with your doctor or vein specialist. It is important to establish a baseline against which progress can be charted. Conservative management of the disease must start early in its course, much earlier than most people realize. Measures must be aimed at countering the effects of gravity and poorly functioning one-way valves which leads to the propensity of the legs to hold onto extra fluid (pooling).
It is important measures that encourage circulation into our daily routines. And best of all, behavior modification doesn’t cost anything.
Graded compression therapy will combat stretching of the veins and pooling of blood in the legs. Compression therapy can come in several forms, but the most common is medical grade elastic stockings. These stockings are available by prescription from your doctor or vein specialist. They are a medical device and should not be ordered online without guidance from a physician.
People who are able to modify their behavior and who are comfortable wearing compression stockings can delay the progression of CVI for a long time, even years. If your symptoms persist and interfere with your activities, in spite of conservative management, you may require treatment.
Multiple modalities exist for the treatment of varicose veins. The various treatments can be used alone, but are usually combined in a variety of ways. Today, all of these are performed as outpatient procedures, usually in the doctor’s office, with local anesthesia.
Whichever methods of treatment are performed, behavior modification and the judicious use of compression therapy, will always be the mainstay of therapy and will be valuable tools for a lifetime of vein health.
Vein treatments are performed at our Salem location by Rick Pittman, MD, board certified in venous and lymphatic medicine. For more information or to schedule a consultation, call 503-362-8385.